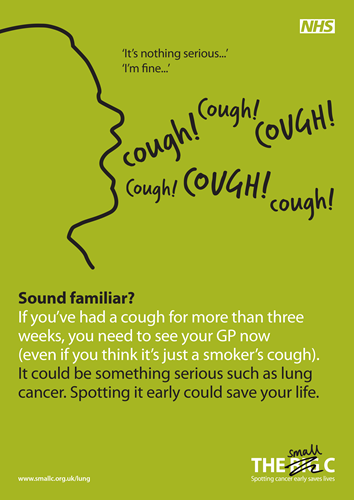
I’ve got a cough that won't go away, what should I do?
If you’ve had it for three weeks or more, or if your long-standing cough has changed, make an appointment with your GP as soon as possible. Chances are it’s nothing serious, but if it’s lung cancer, the time to know is now. Why? You’re much more likely to survive early stage lung cancer than late stage lung cancer.
I’ve smoked for years and I’m always coughing. Will my GP really take me seriously?
Yes. If you’ve had a cough for more than three weeks, or if your long-standing cough has changed, please make an appointment with your GP now. Your doctor will make the time to see you; they will ask you questions about your symptoms and medical history and give you a physical examination.
GPs follow national guidelines when referring patients for tests; if you have any of the symptoms required for an urgent chest x-ray and your GP is worried that lung cancer is a possibility, you will be referred to your local clinic or hospital for an appointment within 2 weeks. Your GP may also refer you for blood tests.
I’ve recently noticed that I get out of breath easily, should I be concerned?
If this is something new or has changed recently, please see your GP straight away. Chances are it’s nothing serious, but it’s better to know now.
What questions should I ask my GP?
You are free to ask whatever questions you feel are important to you.
The following questions may be useful. Feel free to print this list and take it with you to your appointment.
Please remember that you can take someone with you to your appointment, this can help you to make sure you ask all the questions you would like to.
What will happen at my GP appointment?
Your GP will ask you questions about your symptoms and medical history and give you a physical examination. GPs follow national guidelines when referring patients for tests; if you have any of the symptoms required for an urgent chest x-ray and your GP is worried that lung cancer is a possibility, you will be referred to your local clinic or hospital for an appointment within 2 weeks. Your GP may also refer you for blood tests and the hospital might arrange for you to have a CT scan.
What are my risks of getting lung cancer?
Lung cancer mainly affects older people. It is rare in people younger than 40, and the rates of lung cancer rise sharply with age. Lung cancer is most commonly diagnosed in people aged 70-74 years.
Although people who have never smoked can develop lung cancer, smoking causes nearly 9 out of 10 cases. This is because smoking involves regularly inhaling well over a hundred different toxic, cancer-causing substances.
How can I reduce my risks of getting lung cancer?
Nearly nine out of 10 cases of lung cancer are caused by smoking, so if you smoke the best way to reduce your chances of getting lung cancer and other serious conditions, is to stop smoking as soon as possible.
However long you have been smoking, it is always worth quitting. Every year that you do not smoke, your risk of getting serious illnesses, such as lung cancer, will decrease. After 10 years of not smoking, your chances of developing lung cancer falls to half that of someone who smokes.
NHS Smokefree can offer free advice and encouragement to help you quit smoking. You can call them on 0300 123 1044, or visit their website. Your GP, pharmacist or local Stop Smoking provider can also give you help and advice about giving up smoking. Click here to find out more about your local Stop Smoking provider.
In general, maintaining a healthy weight, staying within government guidelines on alcohol, eating a healthy, balanced diet and keeping active can help reduce your risk of some cancers and heart disease. Find out more information about diet and cancer from Cancer Research UK, Macmillan, and the NHS.
Can I be routinely screened for lung cancer?
At the moment there is no national screening programme for lung cancer in the UK. The UK Health Technology Assessment programme is currently assessing tests that could be used to screen for lung cancer. You can find detailed information about research into lung cancer screening from Cancer Research UK.
How is lung cancer diagnosed?
If your GP is concerned about the symptoms you have presented they will arrange for further tests at hospital or urgent referral to a specialist within 2 weeks.
Initially these tests are likely to include:
If these scans show that there might be cancer in your lungs you will be referred for a biopsy (where a small sample of tissue is taken from the abnormal area) which can be carried out in a number of ways, including bronchoscopy. You may also need to have another type of scan called PET-CT scan which helps assess whether the cancer has spread beyond its original site.
What are the treatment options for lung cancer?
If it is found that you do have cancer your treatment will depend on your individual circumstances, such as what type of cancer you have and the stage of cancer.
A specialist team will put together an individual plan for your treatment which could include:
For more information on the treatment of lung cancer click here.